Coronary artery disease
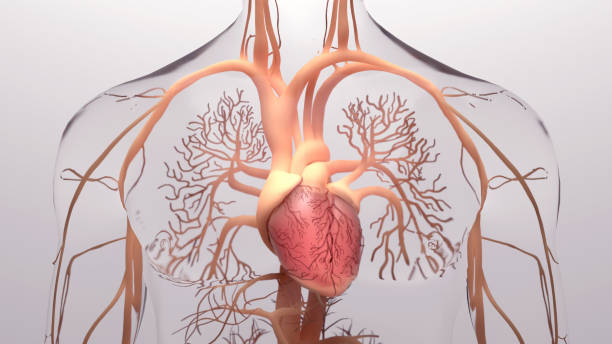
This is one of the most common diseases of the cardiovascular system, characterized by the narrowing or blockage of the coronary arteries that supply blood to the heart muscle. Itis an alarming health condition that affects millions of people worldwide. The narrowing or blockage of the coronary arteries, which supply oxygen-rich blood to the heart muscle, puts individuals at an increased risk of heart attacks and other cardiovascular complications. However, looking beyond its prevalence and symptoms, we uncover a fascinating interplay between genetics and lifestyle factors in the development of this disease.
Recent studies have shed light on the role of genetics in predisposing individuals to coronary artery disease. Various gene mutations have been identified that increase the likelihood of developing this condition, highlighting the importance of early genetic testing for those with a family history. Furthermore, researchers have started to unravel how certain lifestyle factors can modify these genetic influences. Engaging in regular exercise, maintaining a healthy diet, and managing stress levels not only help prevent or delay the onset of coronary artery disease but also mitigate its impact by influencing gene expression.
With such insights into the intricate connection between genetics and lifestyle choices, there arises a new potential for personalized treatment approaches in combating coronary artery disease. By identifying specific gene variants in individuals with heightened risk factors and designing tailored interventions based on their unique genetic profiles, medical professionals can now provide more targeted care strategies. This emerging field holds immense promise not only for preventing future cases but also for enhancing treatment outcomes by addressing individual variations in patients’ responses to medication or procedures.
In conclusion, while coronary artery disease remains one of the most prevalent conditions affecting our cardiovascular system today, advancements in scientific research continuously expand our understanding beyond
Hypertension
Also known as high blood pressure, hypertension puts strain on the heart and blood vessels, increasing the risk of heart disease and stroke.
Hypertension is the silent killer lurking within our bodies. It affects millions of people worldwide, yet many are unaware of its presence until it’s too late. Often referred to as a silent disease, hypertension typically shows no symptoms in its early stages, making it even more dangerous. The first sign is usually a catastrophic event like a heart attack or stroke, leaving individuals and their loved ones bewildered and devastated.
This chronic condition puts an immense strain on the heart and blood vessels, leading to an increased risk for heart diseases such as coronary artery disease or congestive heart failure. With each beat of the heart, blood is forcefully pushed against the walls of the arteries. Over time, this constant pressure damages these delicate structures, causing them to become rigid and less elastic. As a result, additional stress is placed on the heart’s already burdened muscles as they struggle to counterbalance this resistance.
The consequences of hypertension extend far beyond just cardiovascular problems. Studies have shown that high blood pressure also increases the risk of stroke by damaging blood vessels in the brain. Furthermore, it can lead to kidney damage by impairing proper blood flow through these vital organs. Hyperlipidemia (high cholesterol levels) often accompanies hypertension and together they create a deadly combination that furthers our risk of developing other diseases.
It’s crucial for us all to be aware of hypertension’s dangers and take proactive steps towards prevention and management measures such as regular exercise, maintaining a healthy weight and diet low in sodium intake while high in fruits
Heart failure
This condition occurs when the heart is unable to pump enough blood to meet the body’s needs. It can be a result of various underlying cardiovascular diseases.
Heart failure is a condition that affects millions of people worldwide and is often a result of various underlying causes. One of the primary reasons for heart failure is coronary artery disease, where the arteries supplying blood to the heart become narrow and can no longer deliver sufficient blood flow. Another common cause is high blood pressure, which puts excessive strain on the heart’s pumping ability over time.
It’s important to note that heart failure doesn’t mean the heart has stopped working altogether; instead, it means that its efficiency has significantly decreased. This can lead to a range of symptoms such as fatigue, shortness of breath, and fluid retention. While medication and lifestyle changes can help manage these symptoms and slow down disease progression, heart transplantation may be necessary in severe cases.
Additionally, certain conditions like diabetes, thyroid disorders, or infections can also contribute to the development of heart failure. It’s crucial for individuals with these underlying conditions to closely monitor their cardiovascular health and work with their healthcare providers to minimize their risk factors for developing heart failure. By understanding both the common causes and lesser-known contributing factors of this condition, individuals can stay proactive in preventing or managing this potentially life-threatening disease.
Arrhythmias
These are abnormal heart rhythms that can range from harmless to life-threatening. They can cause palpitations, dizziness, fainting, or even sudden cardiac arrest.
Arrhythmias, the irregular and abnormal heart rhythms, may often be underestimated by those who consider them harmless. However, these conditions can range from being a mere inconvenience to causing life-threatening consequences. Understanding the different types of arrhythmias is crucial in order to determine their severity and potential impact on one’s health.
Palpitations are a common symptom experienced when the heart beats irregularly or too fast. While they may be unsettling, most palpitations are harmless and temporary. They can result from stress, anxiety, caffeine intake, or even certain medications. Nonetheless, it is essential not to dismiss persistent or severe palpitations as they could be indicative of a more significant underlying issue.
Dizziness and fainting are alarming signs that should never be ignored when experiencing an arrhythmia. These symptoms occur because of inadequate blood flow to the brain during episodes of abnormal heart rhythms. Fainting spells caused by arrhythmias raise concerns about syncope (loss of consciousness) due to reduced oxygen supply to vital organs including the brain—making it imperative for anyone experiencing such symptoms to seek prompt medical attention.
It’s important not only for individuals with known cardiovascular problems but also for those without any history of heart issues to pay close attention to any unusual sensations in their chest area—particularly if accompanied by dizziness or loss of consciousness—to ensure early detection and intervention for any potentially dangerous arrhythmias that may arise.
Atherosclerosis
Atherosclerosis is a silent killer, often lurking in the shadows and only revealing itself when it’s too late. This insidious disease quietly builds up plaque in our arteries, restricting blood flow and putting us at risk for heart attacks and strokes. While many of us may think that atherosclerosis only affects older adults, the truth is that it can start developing as early as childhood or adolescence.
One of the startling aspects of atherosclerosis is its connection to seemingly unrelated conditions. Research has shown that chronic inflammation plays a crucial role in the development of this disease. In fact, certain inflammatory cells present in other parts of our body can migrate into our artery walls, setting off a cascade of events leading to plaque formation. This means that individuals with chronic conditions like diabetes or autoimmune disorders may unknowingly be at higher risk for developing atherosclerosis.
Moreover, recent studies have shed light on how our lifestyle choices contribute to the progression of this deadly disease. We all know that smoking damages our lungs, but did you know it also accelerates the hardening of our arteries? The chemicals in tobacco smoke not only increase inflammation but also damage the cells lining our blood vessels, making them more susceptible to plaque buildup. Similarly, poor diet choices high in saturated fats and cholesterol contribute to increased cholesterol levels circulating in our bloodstream – fueling the formation of plaques.
Understanding these connections allows us to take proactive steps toward preventing or managing atherosclerosis. Adopting healthier lifestyles through regular physical activity and balanced diets low in